There is no US federal legislation regulating SPHM, but nine states have active laws dictating some form of SPHM policy.
States with active SPHM legislation. (Note, Ohio and Missouri passed legislation that has been repealed).
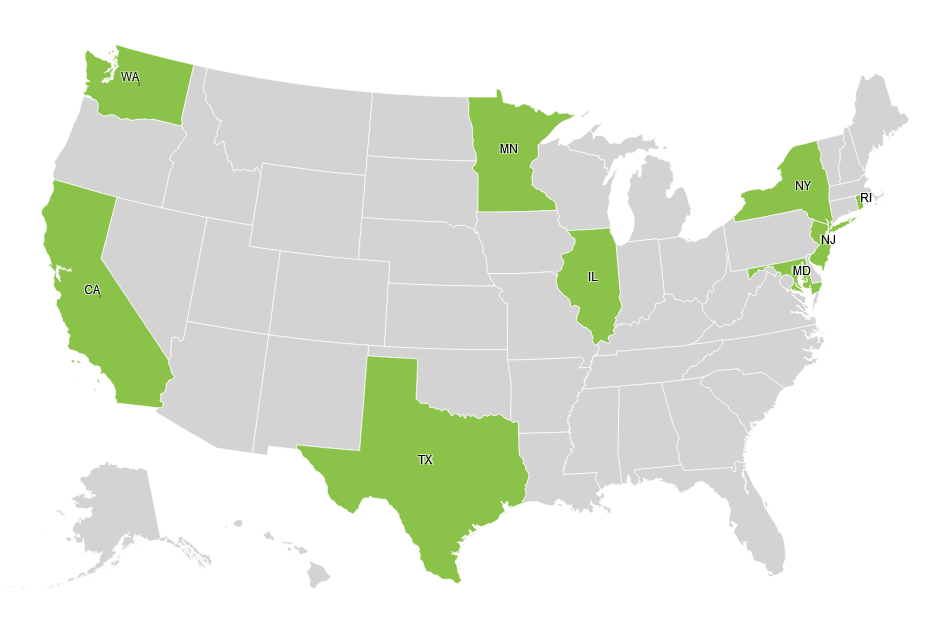
Image courtesy of MonQcle, a project of the Temple University Beasley School of Law’s Center for Public Health Law Research: https://monqcle.com/
Although the policies across states vary, they share similar limitations. The states have sparse or no mandates for SPHM equipment, little funding for acquiring equipment, and little to no mechanisms for enforcement. (See chart below).

Comparison of components of state SPHM statutes. *Legislation has been repealed. Current as of 2022. Courtesy of Adam Moskowitz
Definitions
Hazard Assessment: Evaluations of the patient population and their mobility needs
Safety Training: To ensure workers understand lift equipment and procedures
SPHM Committees: Worker/management entities for determining specific SPHM policies
Refusing Unsafe Lifts: Workers can follow policy without fear of retaliation
Lift teams: Trained specialists for operating SPHM equipment
Funding: Grants or loans for employers to acquire SPHM equipment
New Facility Construction: Meet the physical needs of SPHM equipment in new buildings
The workplaces covered by the state laws are heavily focused on higher acuity settings such as hospitals. Outpatient, assisted living, and group homes have little to no coverage.
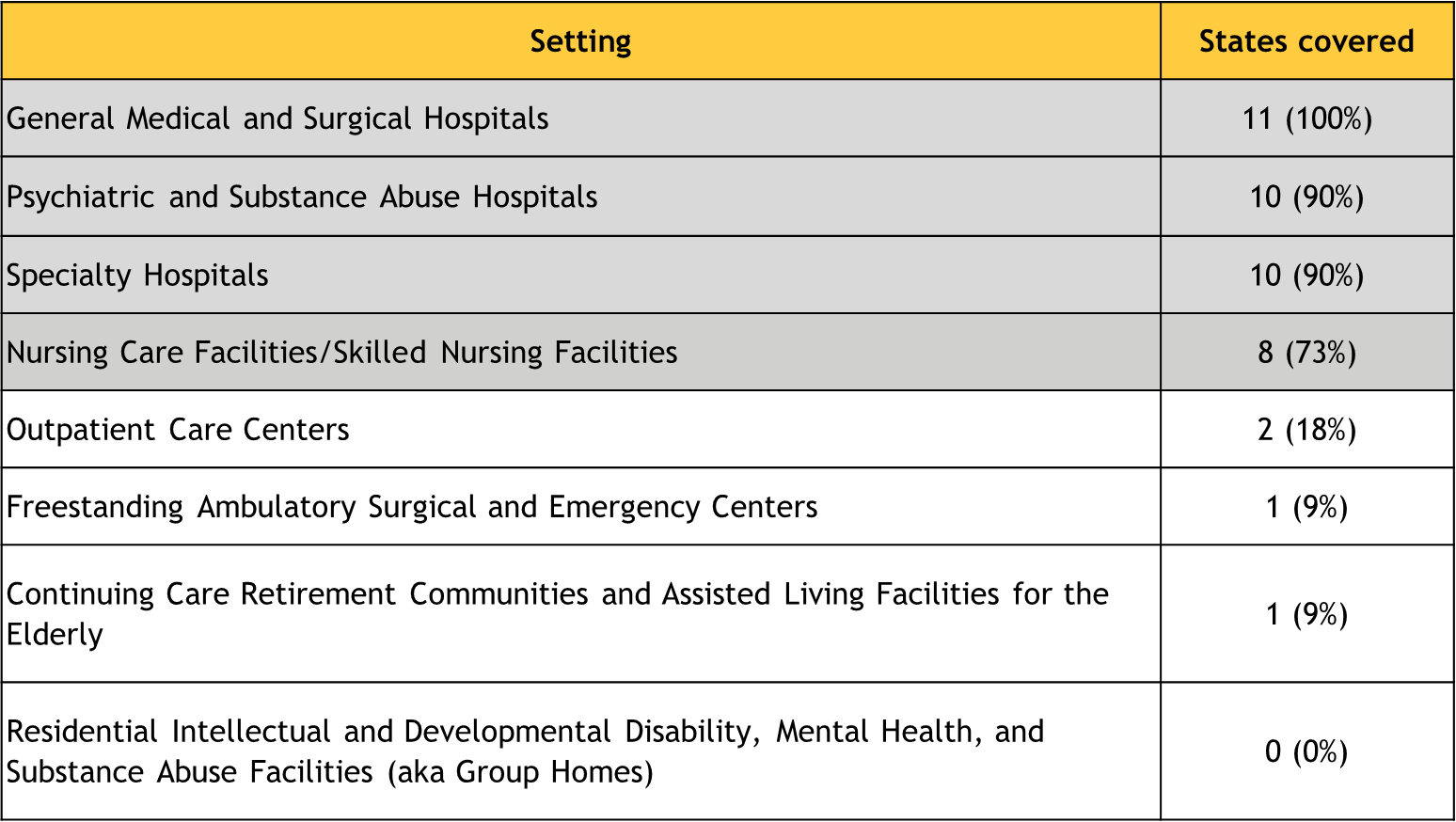
Settings considered in US state legislation. Gray shading represents higher acuity settings. Includes Ohio and Missouri legislation that has been repealed. Courtesy of Adam Moskowitz
Legislation is Effective.
Despite the limitations of the state laws, they do appear to be effective at promoting the use of lift equipment and reducing injuries in healthcare workers. Kayser et al. (2020) found that patients in states with SPHM legislation were 60% more likely to be moved with a lift than patients in other states. Moskowitz (2024) showed that patient handling injuries for healthcare workers in occupational settings covered by Minnesota’s SPHM legislation declined more rapidly than for healthcare workers in settings not covered by the law.
References:
Kayser, S. A., Wiggermann, N. E., & Kumpar, D. (2020). Factors associated with safe patient handling practice in acute care and its relationship with patient mobilization: A cross-sectional study. International Journal of Nursing Studies, 104, 103508. Journal Site
Moskowitz, A. F. (2024). Patient Handling, Workplace Violence, and Contact-Related Occupational Injury Among Residential Care Workers (Doctoral dissertation, University of Minnesota). PDF

